Health Education Services Program for Internal Medicine Residency in Indiana
Becoming a skilled and compassionate physician starts with the right training. With a strong focus on comprehensive learning, the health education services program for internal medicine residency in Indiana offers a well-rounded experience. This article explores the structure, benefits, and future of this innovative residency training approach.
Understanding the Fundamentals
The foundation of any successful medical career lies in effective education. The health education services program is a structured initiative that supports residents through knowledge building, clinical experience, and mentorship. It’s especially critical in internal medicine residency programs across Indiana, where healthcare needs are diverse and complex.
These programs have evolved over the years to incorporate modern technology, research, and interdisciplinary teamwork, transforming how physicians are trained today. This evolution is not only necessary but vital for future healthcare improvements.
1.1 Curriculum Design and Scope
The curriculum in Indiana’s internal medicine residency programs is competency-based and aligns with national ACGME standards. It emphasizes evidence-based practice, patient safety, and interprofessional collaboration. Residents undergo rotations in primary care, hospital medicine, subspecialties, and critical care.
Hands-on simulations and didactic lectures ensure comprehensive exposure. This diverse framework prepares residents to manage both acute and chronic illnesses across populations. Common misconceptions that the curriculum is too theoretical are dispelled through practical applications in real-world settings.
1.2 Mentorship and Clinical Supervision
Unlike other training models, Indiana’s approach incorporates longitudinal mentorship. Faculty physicians not only supervise but guide residents through personal and professional development. These relationships build confidence and accountability.
Mentorship extends beyond clinical duties, helping residents navigate research projects, presentations, and career planning. It’s this dynamic environment that makes Indiana’s health education services program unique and highly effective.
Practical Implementation Guide
Applying the principles of health education in residency settings requires structure and commitment. In Indiana, residency coordinators and hospital partners work together to deliver consistent, high-quality learning. Residents can expect structured timelines, performance evaluations, and feedback loops that enhance growth.
2.1 Actionable Steps
- Step 1: Apply to an accredited internal medicine residency in Indiana that integrates health education services. Review program components to align with career goals.
- Step 2: Leverage hospital-based learning tools, such as electronic health records, simulation labs, and online learning portals.
- Step 3: Follow a clear roadmap: 1st year (foundations), 2nd year (advanced clinicals), 3rd year (leadership & electives). Attend monthly evaluations to stay on track.
2.2 Overcoming Challenges
Common obstacles include:
- Information overload — Mitigated through scheduled reviews and study groups
- Burnout — Addressed by wellness programs and work-life balance modules
- Complex patient loads — Managed with team-based care strategies and case conferences
Residents are encouraged to seek peer support, utilize mental health services, and maintain open dialogue with supervisors. Institutions often assign wellness coaches to ensure sustainable performance.
Advanced Applications
Once residents master foundational skills, they transition into more complex, real-time clinical leadership roles. These advanced applications refine both their medical expertise and system-level thinking. Indiana programs promote innovation and specialization to foster career-long learning.
3.1 Specialized Research and Case Studies
Residents have the opportunity to engage in scholarly activities such as publishing research, leading quality improvement projects, and attending national conferences. Many institutions partner with universities and public health entities to enrich these experiences.
For example, one Indiana resident led a diabetes care model redesign that reduced patient readmission rates by 25% in six months. Metrics like patient outcome data and procedural proficiency track progress effectively.
3.2 Integrative Healthcare Models
Advanced training often involves cross-disciplinary work with pharmacists, psychologists, and social workers. This prepares residents for real-world care coordination.
Compatibility is key, especially in value-based care settings. The program helps residents adapt their clinical judgment across multiple environments — from urban hospitals to rural clinics — ensuring broad readiness.
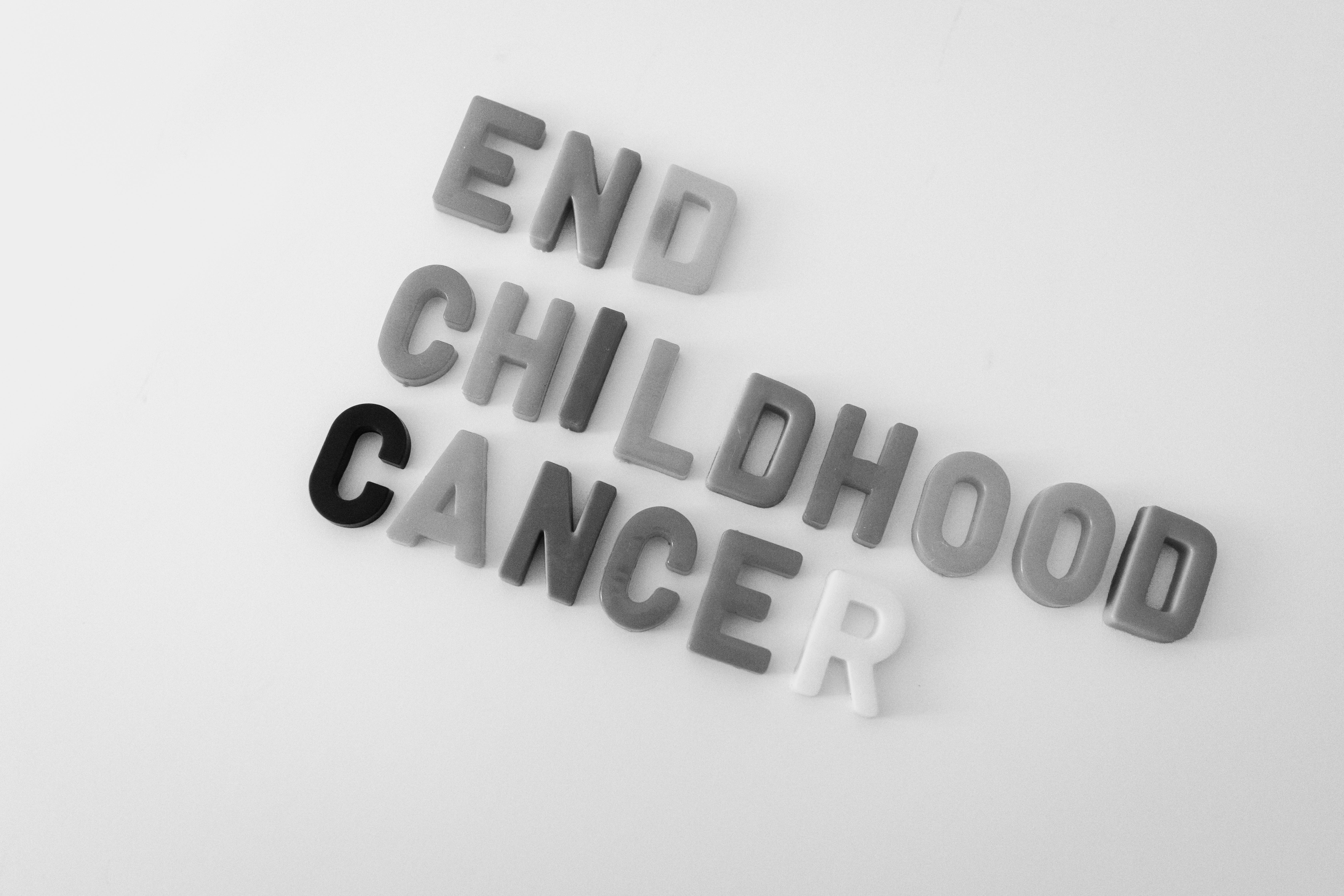
Future Outlook
The future of health education services programs in Indiana looks promising. Emerging trends include AI integration in diagnostics, virtual reality simulations for surgery, and telemedicine expansion. Programs are rapidly adopting these tools to stay ahead of national standards.
Over the next five years, experts predict a stronger focus on preventive care, interdisciplinary teaching models, and international collaboration. Prospective residents can prepare by strengthening tech skills and staying informed on global health trends.
Conclusion
To summarize:
- The health education services program supports internal medicine residency through structured, competency-based training.
- Mentorship, advanced learning tools, and practical experience shape well-rounded physicians.
- Future innovations promise to elevate the quality of care delivered by Indiana-trained doctors.
If you’re passionate about internal medicine, Indiana’s programs offer an exceptional launchpad. Take the next step by exploring accredited residency options and preparing your application portfolio. This is your opportunity to make a real difference in patient care and medical leadership.
Frequently Asked Questions
- Q: What is a health education services program? It’s a structured learning system that enhances medical residency training through mentorship, resources, and hands-on practice.
- Q: How do I start an internal medicine residency in Indiana? Apply through the ERAS system to programs in Indiana, ensuring your application aligns with their health education framework.
- Q: How long does internal medicine residency take? Typically, it spans three years, with potential for subspecialty fellowship afterward.
- Q: What are the costs involved? While residents earn stipends, costs may include housing, board exams, and educational materials. Some programs offer financial aid.
- Q: How does this compare to other states’ programs? Indiana stands out for its hands-on approach, community-focused training, and integration of emerging technologies.
- Q: Is the program technically challenging? Yes, but support systems like coaching, mentorship, and simulation labs help manage the learning curve.
- Q: Can this apply to rural healthcare? Absolutely. Indiana’s residency programs often include rotations in rural areas to prepare residents for a variety of care settings.